
Spine Disorders Treatments
- Low Back Pain
- Sciatica (Lumbar Radiculopathy)
- Neck Pain
- Cervical Radiculopathy
- Lumbar Disc prolapse (Disc Herniation)
- Spinal Canal Stenosis
- Spondylolisthesis
- Osteoporotic spine fractures
- Fractures of Spine
Low Back Pain

Your back is formed by bones, muscles, nerves, and ligaments that work together to help you stand and bend. Between each stacked pair of bones (vertebrae) in the spinal column is a disc acting like cushions.
Nonspecific back pain – This type of pain most often represents a strain in one or more of the muscles in the lower back, and it can be severe.
Serious potential causes — Rarely, back pain is caused by a potentially serious spinal condition, such as an infection, tumour, or “cauda equina syndrome,” which causes leg weakness and bowel or bladder dysfunction as well as back pain.
Degenerative disc disease — Over time, normal wear and tear can lead to degenerative disc “disease” (breakdown of the spinal discs), with the development of small cracks and tears and/or loss of fluid in the discs.
Bulging and herniated discs — Too much wear and tear on spinal discs can lead to the bulging of a disc, in which the outer covering is weakened and the disc protrudes. Some people may develop sciatica (pain that extends down the back of the leg) if the bulging disc presses on a nerve.
Osteoarthritis — Osteoarthritis can affect the joints that connect the vertebrae to one another, called the facet joints. This condition, known as facet joint arthropathy, can lead to bone spurs around the joint and may cause low back pain.
Treatment: Unless the low back pain is caused by a serious medical condition, it typically resolves fairly quickly. Most of the patients can be managed with a short period of relative rest, activity modifications, physical modalities, analgesics, muscle relaxants and physiotherapy exercises. Only a small minority of people with low back pain will require surgery.
Sciatica (Lumbar Radiculopathy)
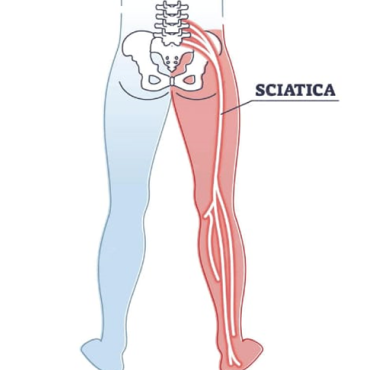
Sciatic nerve starts in the lower back and runs down the back of each leg. The nerve controls the muscles in the lower leg and provides sensation to the back of the thigh, lower leg and the sole of your foot. Sciatica is the term given to the pain, numbness or tingling sensation radiating along the course of the nerve. Severe cases of sciatica present with muscle weakness. Common causes for sciatica include irritation of the sciatic nerve roots due to herniated disc in lumbar region, bony overgrowth or stenosis from degenerative disorders in lumbar spine, compression of the nerve under piriformis muscle in the buttocks.
Neck Pain
The neck or cervical spine is formed by seven cervical vertebrae bone C1 to C7. In between adjacent vertebra are discs, which act as shock absorbers. There are supporting ligaments and muscles.
Causes of Neck pain include: Cervical strain (injury to the muscles of the neck, causing tightness of the cervical and upper back muscles), Cervical spondylosis (wear and tear of the cervical spine),
Cervical facet osteoarthritis, Whiplash injury (traumatic event that causes an abrupt forward/backward movement of the neck). In most cases, neck pain can be treated conservatively
with medications, ice or heat, and stretching exercises and postural corrections. Surgery may be recommended for those with symptoms related to nerve or spinal cord compression (cervical
spondylotic myelopathy or cervical radiculopathy).
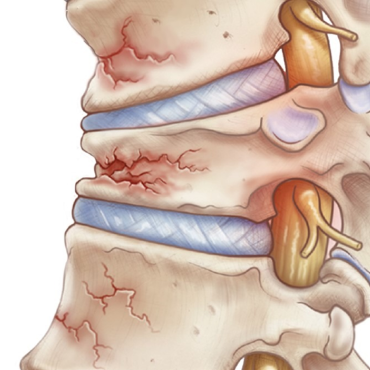
Cervical Radiculopathy
Cervical radiculopathy means that a nerve in the neck (a cervical nerve) is pinched. This can happen because of an injury to the cervical spine (vertebrae) in the neck, or due to age related degeneration
of the cervical disc. This condition can cause pain or loss of feeling (numbness) that runs from your neck all the way down to your arm and fingers. With rest, the condition often gets better over time.
Treatment includes soft neck collar for short periods of time, doing exercises to strengthen your neck muscles and medications. Surgery may be needed if other treatments do not help. The type of
surgery that is used will depend on the cause of your condition.
Lumbar Disc prolapse (Disc Herniation)
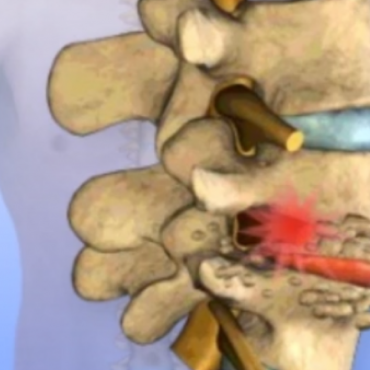
Healthy discs work like shock absorbers to cushion the spine. They protect the spine against the daily pull of gravity. They also protect it during strenuous activities that put strong force on the spine, such as jumping, running, and lifting.
Herniation occurs when the nucleus in the centre of the disc pushes out of its normal space. The nucleus presses against the annulus, causing the disc to bulge outward. Sometimes the nucleus herniates completely through the annulus and squeezes out of the disc.
Spinal Canal Stenosis

Spinal stenosis describes a clinical syndrome of buttock or leg pain. These symptoms may occur with or without back pain. It is a condition in which the nerves in the spinal canal are compressed. The spinal canal is the hollow tube formed by the bones of the spinal column. There are many reasons why symptoms of spinal stenosis develop. Some of the more common reasons include congenital stenosis (being born with a small spinal canal), spinal degeneration, spinal instability, disc herniation. Treatment: Unless your condition is causing significant problems or is rapidly getting worse, it can be managed with nonsurgical treatment. Surgery is recommended for those with neurological decline.
Spondylolisthesis
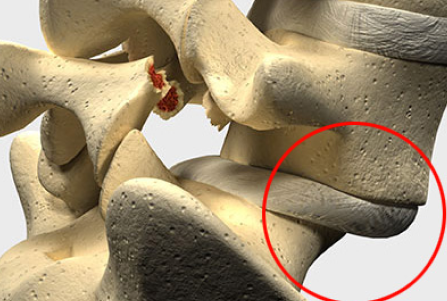
Normally, the bones of the spine (the vertebrae) stand neatly stacked on top of one another. In this condition, one of the spine bones slips forward over the one below it. As the bone slips forward, the nearby tissues and nerves may become irritated and painful. An ache in the low back and buttock areas is the most common complaint in patients with spondylolisthesis. Nerve compression can cause symptoms where the nerve travels and may include numbness, tingling, and muscle weakness in the legs. Most patients with symptoms from degenerative spondylolisthesis do not need surgery and respond well to nonoperative care. Medications may be prescribed to help ease pain and muscle spasm. A rigid back brace for two to three months is recommended for those with pars fracture. Surgery is used when the slip is severe and when symptoms are not relieved with nonsurgical treatments.
Osteoporotic spine fractures
Osteoporotic spine fractures are a common and serious condition where weakened bones in the spine break, due to osteoporosis. These fractures can cause severe back pain, reduced mobility, and a decrease in quality of life. Typically occurring in older adults, especially postmenopausal women, these fractures happen from minor injuries. Treatment options include medications to strengthen bones, pain management, physical therapy, and in severe cases, procedures like vertebroplasty or kyphoplasty.
Spine Fractures
Spinal fractures anywhere along the spine mostly result from serious injuries like high-energy trauma. Spinal fracture symptoms may include: Pain in the back or neck, Tingling or numbness in limbs, Weakness or paralysis of limbs, Uncontrolled muscle contractions, Loss of urinary or bowel control. It requires an evaluation on emergency basis. When a spinal fracture is suspected, the first step is to stabilize the individual. This may be done through the use of a backboard, stretcher or cervical collar to prevent the person from moving and sustaining further injuries. Minor fractures of the spine can be managed with rest and medication. Whereas more severe fractures might require surgery to realign the bones. If left untreated, spinal fractures can lead to permanent spinal cord injury, nerve damage and paralysis.

